Data Findings: Critical staffing lessons for the NHS
COVID-19 has undoubtedly been the biggest challenge faced by the NHS in a generation; a challenge which continues to evolve and to drive innovation.
With a second wave of infection now spreading across Europe, the government and the NHS are once again gearing up to cope with a period of intense demand. However, we are in a very different place from where we were in March. Thanks to the experience, hindsight, and a better scientific understanding of the virus, we now have a wealth of powerful knowledge. This is the weapon which the NHS must use to deliver an effective response this winter.
Using the Patchwork Health live data analytics platform, Patchwork Insights, we have collected and analysed a wealth of data from our partner hospitals. The emergent patterns and clear trends are lessons to be learned, lessons which will be invaluable to Trusts looking to effectively manage their temporary staffing over the coming months
Below, our Data Team has summarised the most important lessons which NHS staffing managers must take forward from the first wave. Our intention is to show that, with the right knowledge and oversight, the NHS can carry the nation through future COVID waves.
Lesson 1: To ensure shift need is met, anticipate the peaks in advance
Because of the lag-time which inevitably accompanies the recruiting and onboarding of staff, periods of intense staff demand must be planned for well in advance. This means that shift request volumes must be increased weeks prior to anticipated peaks in patient intake.
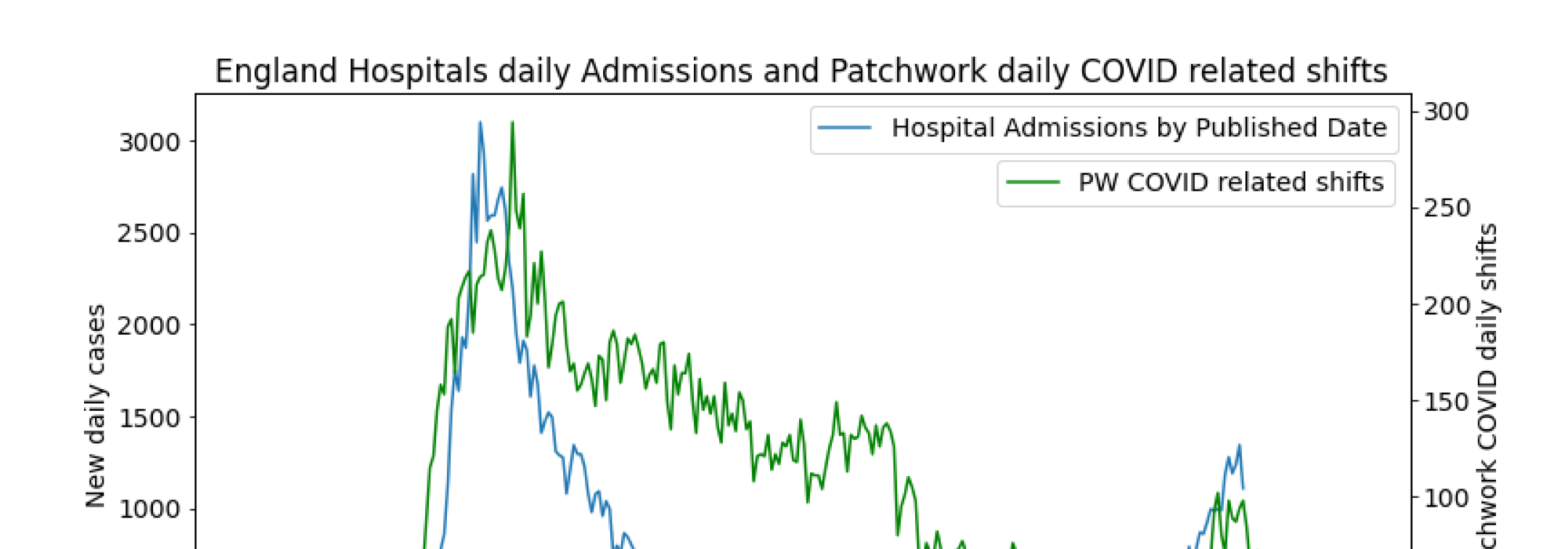
In March, hospitals were largely caught on the back foot when it came to building up their staff numbers. This is hardly surprising, as few would have predicted the rapid uptick in hospital admissions and staff self-isolation rates. Indeed, Figure 1 shows that, on average, hospitals were behind the curve when it came to matching their staffing to the number of patient admissions. The peak in shift requests from hospitals in England occurred after the peak in patient admissions.
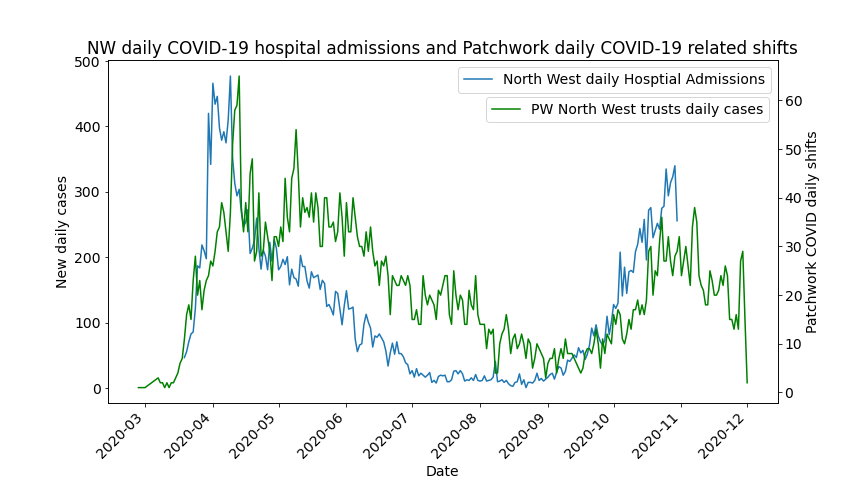
Our data does however show some examples of good practice – Figure 2 shows how in London temporary staff requests were quite tightly aligned to peaks in hospital admissions. In contrast, in the North West the impact of delayed recruitment was more acutely felt, as evidenced by Figure 3.
The lesson which can be taken forward from these graphs is that a forward-looking orientation is crucial for hospital staffing teams. Of course, effective forward planning has always been a priority, but the unique nature of the COVID-19 virus means that it’s a different set of data and trends that need to be monitored. Now that Trusts have February-April data as a benchmark, it’s likely to be easier for them to pre-empt their staffing needs and respond accordingly.
Fig 1. Hospital admissions vs Patchwork Covid related shift requests – UK
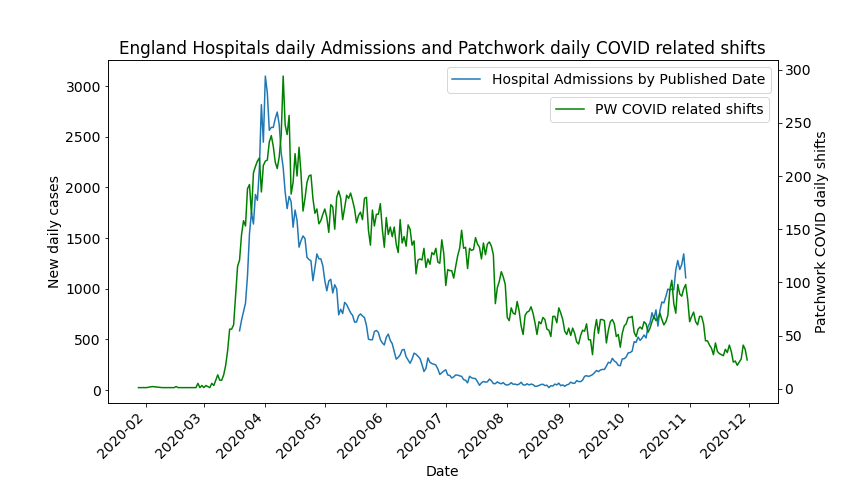
Fig 2. Hospital admissions vs Patchwork Covid related shift requests – London
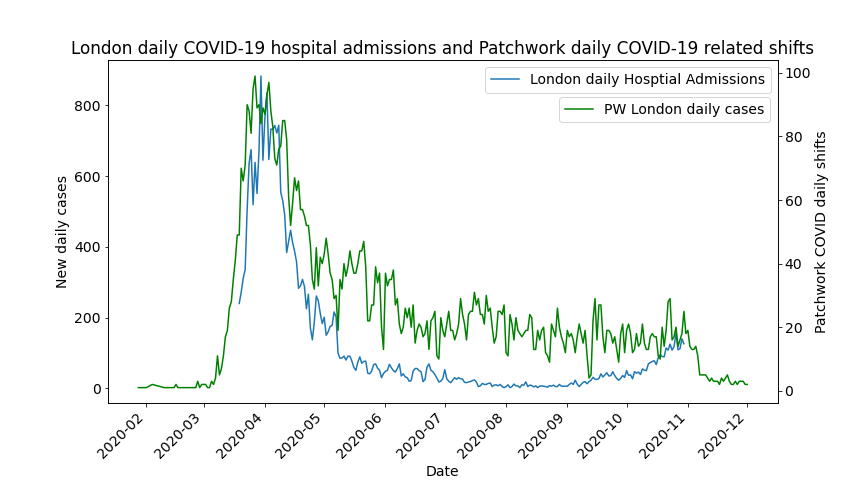
Fig 3. Hospital admissions versus Patchwork Covid related shift requests – North West
Lesson 2: Match staffing capacity to admission peaks
Another key insight which can be gleaned from the latest data is that preparedness must not be misrepresented as over-staffing.
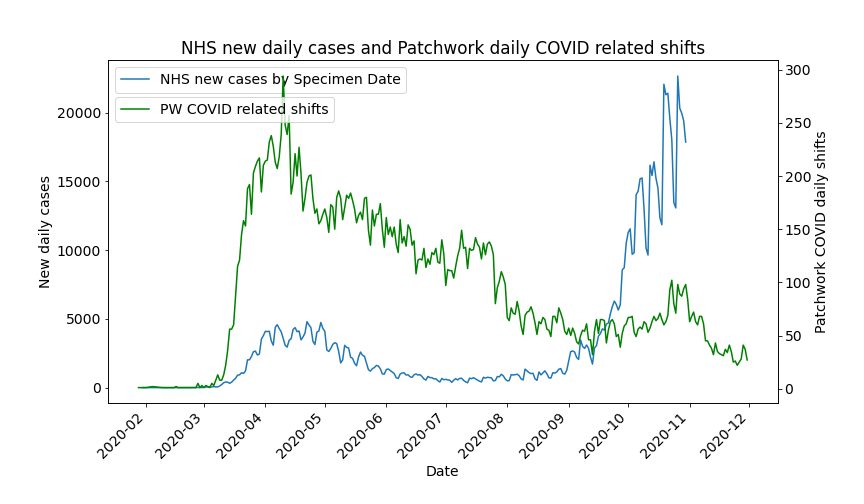
This is easier said than done. In pre-pandemic days, a rise in COVID-related advertised shifts (such as that which Figure 4 shows in July) at a time of falling hospital admissions would have been flagged as an inefficient use of resources.
However, when Figure 5 is taken into account, which shows that a second infection surge began in September, this ‘over-staffing’ can be seen as an example of preemptive capacity building which set the NHS up well to react to the second wave. This capacity building could have in fact been achieved to a much greater extent – the drop in shift requests in August-September later proved to have been over optimistic.
Norms and expectations in the domain of temporary staffing must evolve to reflect the new normal. Capacity building in advance will hurt bottom lines at first, but it will certainly save money, time, and (most importantly) lives further down the line.
Fig 4.
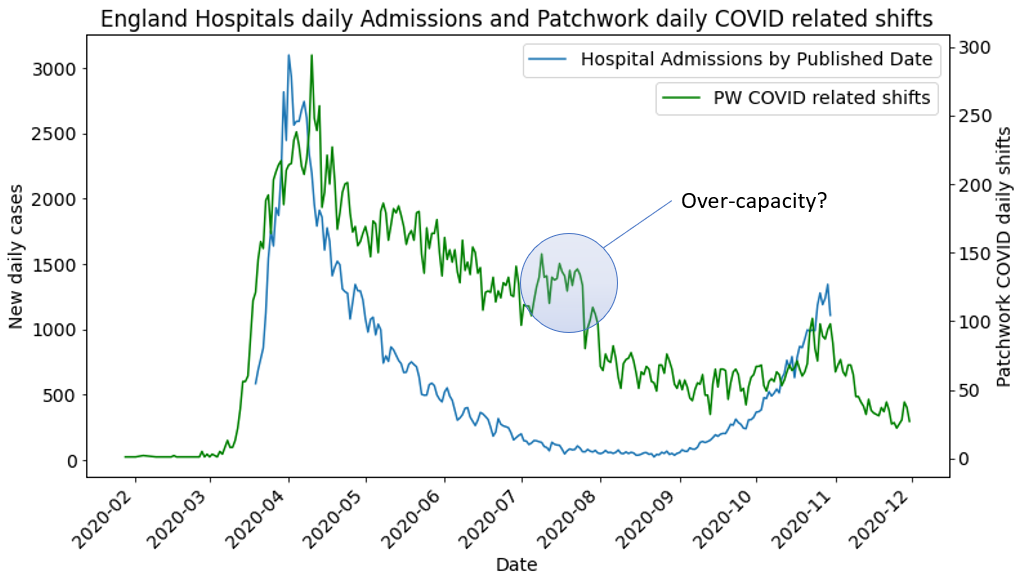
Fig 5.
Lesson 3: Increase shift lead times
Shift ‘lead times’ refers to the number of days’ in advance that shifts were broadcast on the Patchwork platform. In the majority of cases, the longer the lead time, the more likely it is that the shift will be filled.
It’s widely accepted that very short notice shifts are much less likely to be filled, as staff often must make preparations (such as childcare or transportation) in advance if they are to be able to work.
Figure 6.0 shows just how short notice periods for frontline shifts were, during the first peak of the pandemic. The daily number of cases was tightly correlated with a decreasing number of days’ notice given to clinicians (see red trend line on Fig 6.0). Again, this is on account of the unexpected surge in service demand and the high number of staff absences.
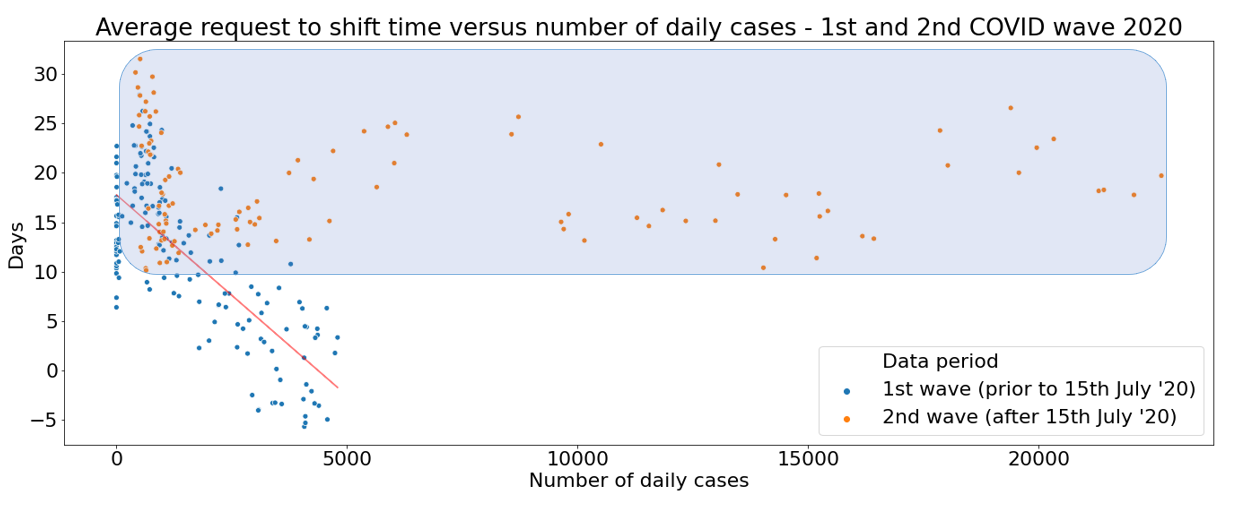
Encouragingly, Figure 6.1 shows that first-wave lessons were taken on board by Trusts when it came to increasing lead times after July 15th. Not a single ‘second wave’ shift was advertised with fewer than 10 days advance notice (as highlighted with the blue shaded area on Fig 6.1). This example of adapting practice in line with insights from collected data will inevitably help to drive up shift fill rates and patient safety outcomes, now and in the future.
Fig. 6.0
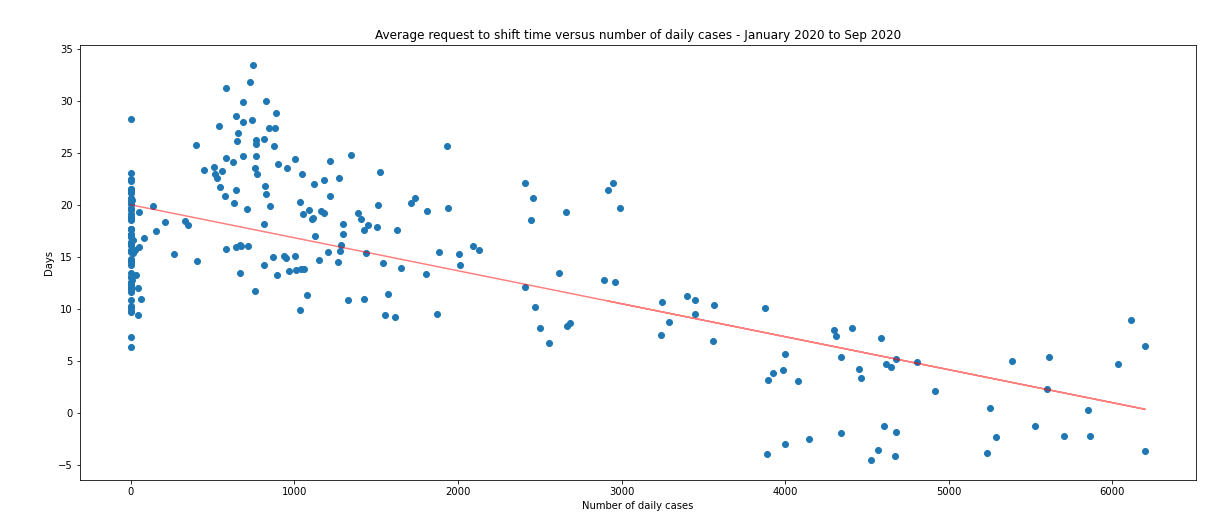
Fig 6.1
Lesson 4: Understand where your clinicians are coming from
As administrators and staffing managers know, clinicians are not interchangeable entities. To ensure that inductions, safeguarding, training and numerous other variable factors are well managed, it’s essential to monitor exactly who is filling each shift in real-time.
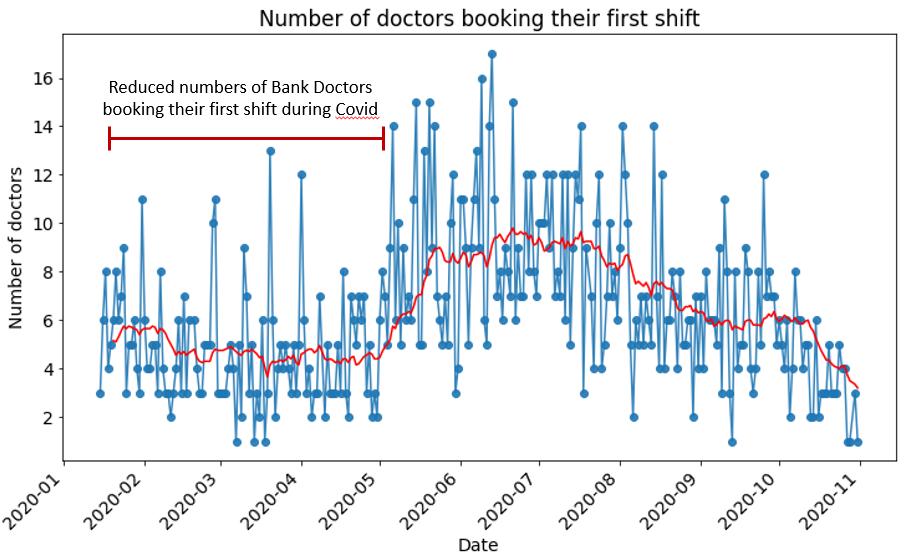
Figure 7 shows significant spikes in the recruitment of new doctors to hospitals during the pandemic spring peak, and another spike at the end of October. However Figure 8 shows that these new recruits have not been booking their first shifts at times of elevated hospitalisation rates.
This suggests that hospitals are continuing to rely on their internal staff banks during periods of high pressure. This is most likely due to the benefits of relying on staff members who are more comfortable with and used to working in that clinical site, do not need inducting and have stronger professional connections with existing teams.
However, this is likely to lead to more complicated problems in the coming months. Unlike in the spring, the majority of hospitals are planning to continue with elective surgery and non-COVID-related procedures throughout the winter. This is an undoubtedly necessary decision, but it does mean that hospitals will not be able to redeploy their existing substantive staff to treat COVID admissions in the way they did in the spring, and so will instead need to utilise these newly onboarded temporary staff instead.
Figures 7 and 8 evidence the need for hospitals to build their temporary staffing reserves in times of (relative) low demand, in order that they are ready to be drawn upon during times of critical need. Similarly, recruits onboarded during demand peaks must be given opportunities for familiarisation and induction when pressures recede, so that they will be more useful to hospitals during later waves. The red trend line on Fig. 8 shows this happening during the late summer months of 2020. This will mean that fewer resources and time need to be expended on recruitment or agency staff when the hospital experiences high demand in the future.
The risk from COVID is not going to abate any time soon, but it’s not too late for hospitals to get their staff banks and associated operations in order. Building a strong internal reserve of known personnel is an investment that will pay dividends.
Fig 7.
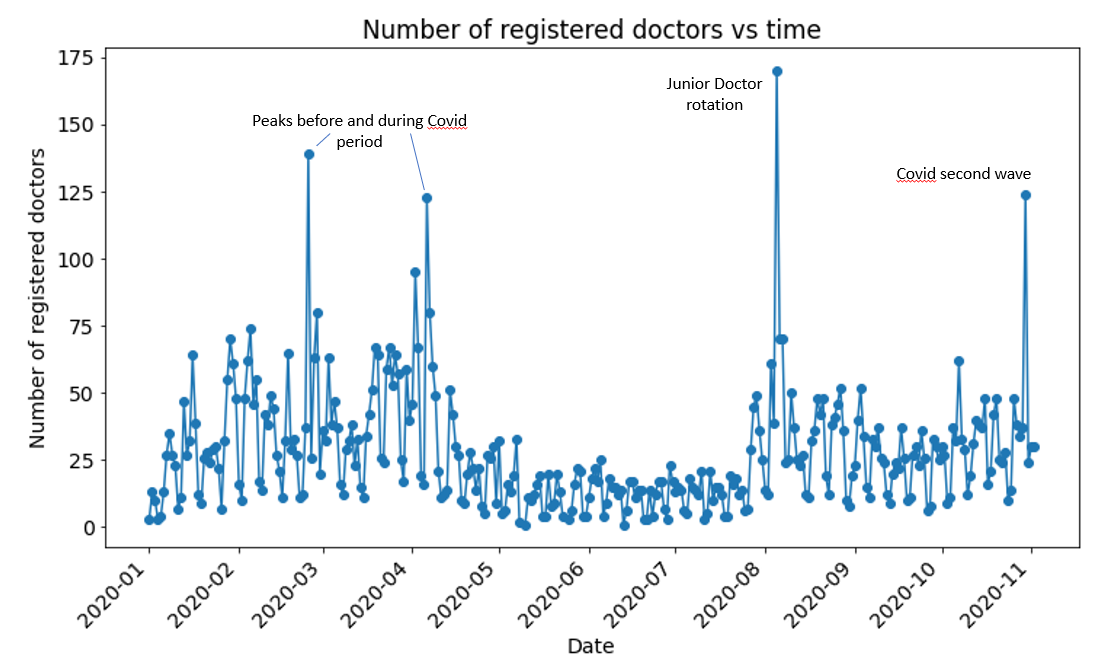
Fig 8.
These four short lessons drawn from country-wide hospital staffing data have a common theme: a forward-oriented, proactive approach is essential to the delivery of successful staffing outcomes.
As the NHS embarks on tackling the second COVID wave, we are fortunate to have the twin benefits of first-hand experience and comprehensive data. The intelligently-interpreted data insights combined with on-the-ground experience of tackling the virus provides NHS Trusts with a head start in the current race.
Patchwork Health are working hard to support our NHS partners in building strong internal staff banks, enabling successful advance shift advertisement and capacity building. Thanks to ongoing collaboration and the incredible commitment of the staff who accept these vital shifts, NHS hospitals will be better-prepared for whatever 2020 and 2021 bring.