Cracking the code on NHS pay rate escalations

Why are we exploring NHS staffing and pay rate escalations?
With the NHS continuing to face intense workforce pressures, managing staffing costs remains a major concern, with rising pay rate escalations cited as a major expense. Our research indicates that organisations are spending an average of £20 extra per hour per shift on rate escalations, with over 20% of all shifts being affected by these increases.
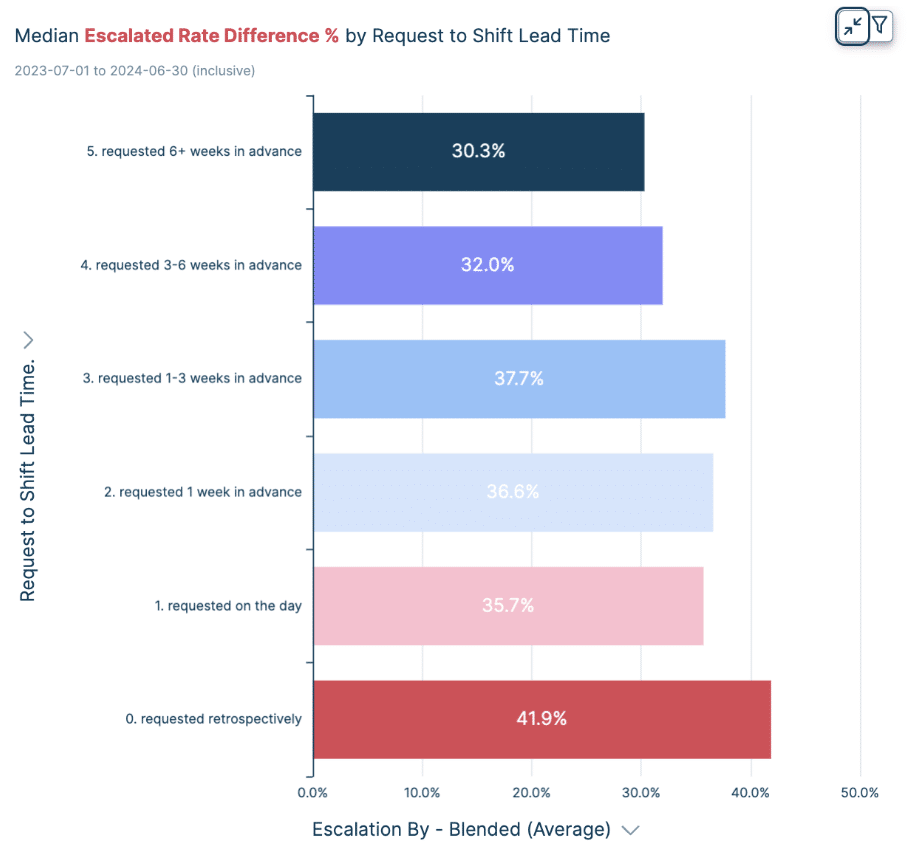
To address this, Patchwork’s data team has delved into the reasons behind these high escalation rates, seeking ways to predict and mitigate them – using reporting tool, Patchwork Insights. The analysis reveals a link between lead times and escalation costs, indicating that shifts booked closer to their start date tend to incur higher expenses.
By understanding these dynamics and leveraging advanced predictive models, NHS trusts can make data-informed decisions to control costs and enhance operational efficiency.
So, how did we go about looking for answers?
At Patchwork, we have a tech team made up of engineers, analysts and NHS staffing experts who have been working with workforce data for years. They have uncovered a wealth of data to identify why high levels of rate escalation arise and methods to reduce them.
Leveraging the power of a neural network model – a sophisticated AI deep learning system inspired by the workings of the human brain – they analysed past data to make these predictions. The model uses interconnected nodes, much like neurons, to process information and forecast potential escalations. The ultimate goal is to alert users as early as possible if a shift is likely to be escalated, giving them the opportunity to act swiftly and secure a better rate.
And what did we find out that can impact NHS staffing?
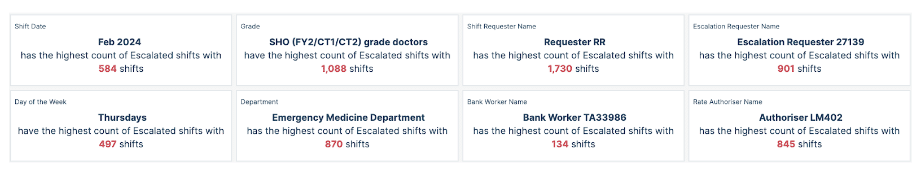
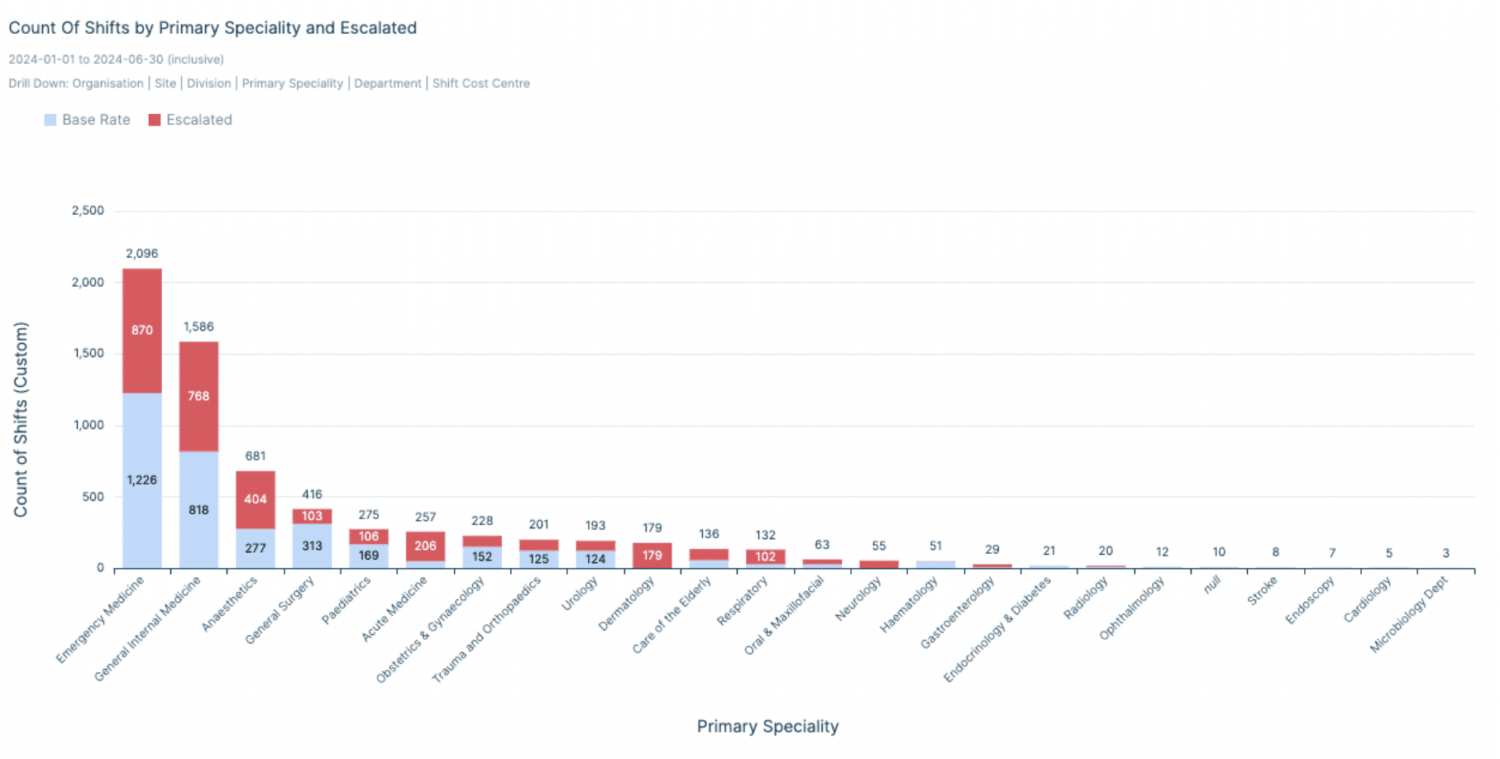
The team uncovered some valuable findings through their research. Their analysis revealed a striking pattern: the shorter the lead time between the request for a shift and the shift’s start date, the higher the rate of escalation. In really simple terms, the closer we get to the shift’s start time, the more likely we are to see an increase in escalations. This is particularly evident with STR 3+ medics: the grade with the highest number of escalated shifts this year.
The analysis has also shown that certain variants are pivotal in predicting whether a shift will be escalated. Factors such as grade, department, and division play a crucial role. Other features like lead time also become significant when examining the rates and the extent of escalation. The initial unsocial rate of a shift was found to be a more critical factor than the initial core rate, even when considering escalation rates for core hours – the team’s analysis shows that this could be down to individuals who tend to focus on the highest figure associated with the shift and base their escalation value on this. For example, if a shift has a higher pay rate for unsocial hours (like nights or weekends) compared to regular core hours, staff might use this higher unsocial rate as a reference point when negotiating or considering escalation rates – which would impact reporting and spend.
When organisations have the data available to gain a greater understanding of when and where these escalations are coming from (as shown in the graphics below), they can dedicate more targeted resources and make informed decisions to minimise the need to escalate shifts at a later stage.
This is just one example of how data can objectively determine problem areas for organisations looking to address NHS staffing spend. Patchwork Insights gives organisations unparalleled access to their data and as we build and create more advanced reporting tools, we’re excited to make more intelligent reporting available to help organisations make better decisions than ever.