How can self-rostering support your NHS organisation and clinicians?
What is self-rostering in the NHS?
Self-rostering refers to the practice of allowing staff to choose the shifts they work, as opposed to a rota coordinator organising each individual’s schedule. This flexible approach to rostering allows clinicians to have more control over their working hours, and is designed to address several challenges associated with traditional rostering, such as work-life balance, staff satisfaction, and retention. It’s important that this flexibility is balanced against service demand, ensuring minimum staffing numbers are achieved for patient safety. When implemented properly, self-rostering can greatly reduce (or in some cases remove) the need for ‘shift swaps’; a process which can be frustrating and time-consuming for both clinicians and rota coordinators.
In traditional self-rostering, whilst clinicians may appear able to choose their preferred shifts, the process typically includes a negotiation element, where team members coordinate to ensure that all shifts are covered appropriately. This might involve negotiations or adjustments agreed between the team members, or changes may be manually made by a rota coordinator to ensure the needs of the service, and more broadly the patients, are met. If clear communication around the process is not properly implemented, clinicians may wrongly assume that their choices are ‘guaranteed’ at the point of choosing their shifts.
If adjustments are then required to ensure safe staffing levels, this can lead to conflicts, confusion and dissatisfaction with the process, with some clinicians feeling they have been treated unfairly. In extreme cases substantive cover may not be achieved, risking safe staffing levels and leading to a greater reliance on additional bank or agency coverage. The process can also be time-consuming for everyone involved, with clinicians having to first select each shift individually and then make time for a meeting to discuss adjustments. Adjustments and negotiations also place a heavy admin burden on rota coordinators.
What are the benefits of self-rostering?
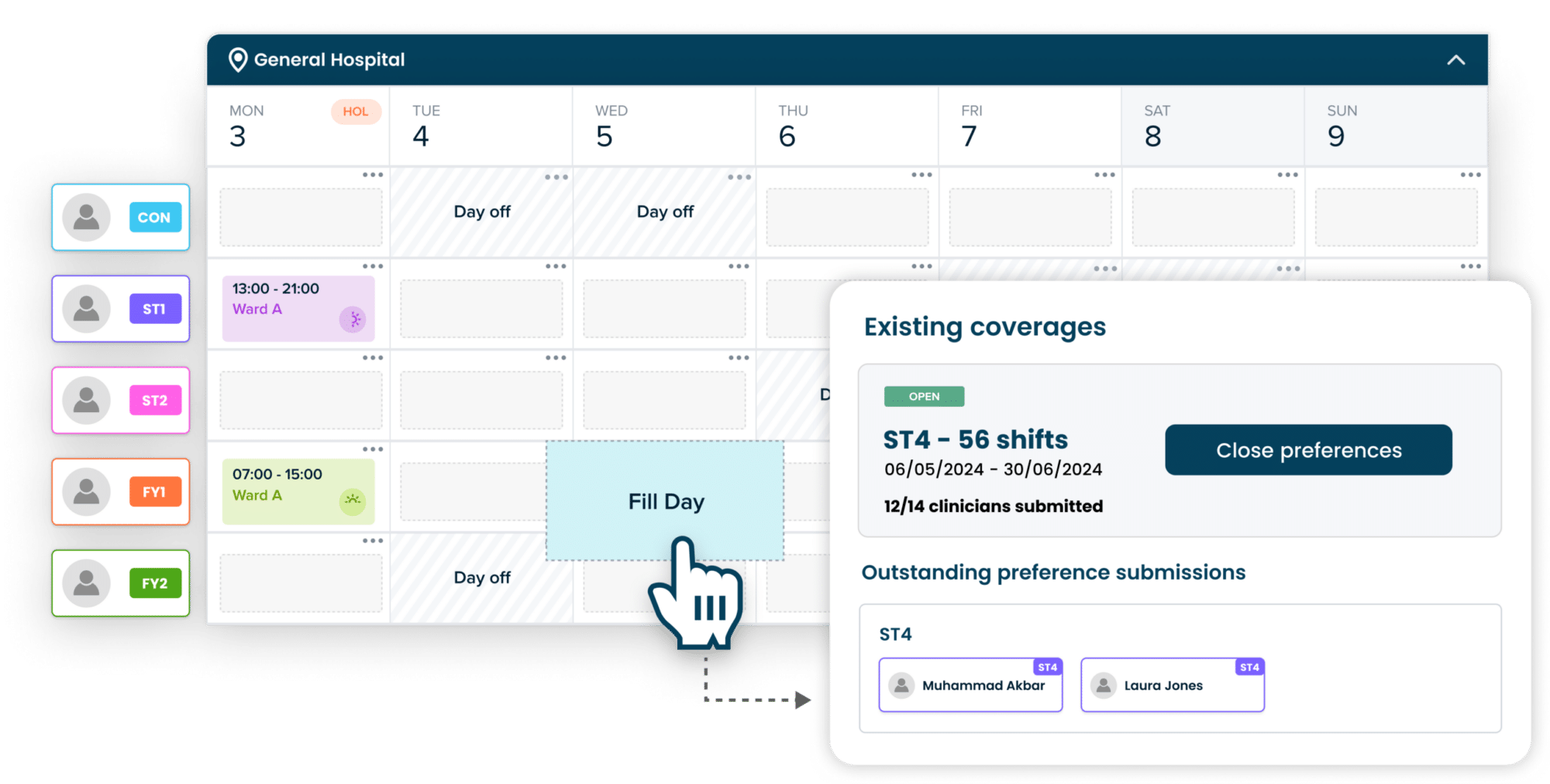
One approach to unlocking the true potential of self-rostering is to take a preference-led approach, making use of a sophisticated algorithm to remove the need for manual adjustments. With this approach, a rota coordinator would send the upcoming roster period out to clinicians to submit their preferences. The window for assigning preferences should be carefully considered and stated at all stages of the process, to ensure fairness and provide maximum clarity. Clinicians should be able to request shifts that best suit their personal and professional needs, including selecting preferred working hours and days off. Once preferences have been submitted, the system should algorithmically assign shifts to each worker based on various factors, including:
- Compliance and regulatory considerations
- Minimum staffing numbers (MSN)
- Scheduled leave and leave requests
- Submitted preferences
Rota coordinators will then be able to adjust allocations before publishing the roster if needed. This approach offers maximum flexibility without compromising on safe staffing or fairness. Clinicians are not required to assign themselves shift-by-shift, or to make time for additional meetings to negotiate adjustments within the team. Rota coordinators also save significant time creating rosters and service managers achieve greater governance to ensure safe staffing for patients. This approach does not work on a ‘first come, first serve’ basis, meaning clinicians don’t feel as though they are competing or need to work towards unrealistic deadlines, fostering good working relationships between clinicians and rostering teams as a result.
Find out more about how Patchwork Rota supports easy, efficient and safe rostering here.