NHS rostering productivity is a frequently discussed topic, and is often highlighted as an area for improvement across all organisations. Workforce productivity refers to making the most effective and efficient use of staffing resource to deliver high-quality, cost-effective and safe patient care. But this can only be achieved with the right tools in place. Many staff are still using outdated rostering software that lacks necessary functionality and reporting capabilities, leading to wasted time and resources. For clinicians, cumbersome systems for requesting leave and managing schedules can lower employee engagement and morale, further hindering productivity.
An effective e-rostering system can address these challenges. To support this in practice, the e-rostering meaningful use standards published by NHSEI provide a framework of five attainment levels, setting benchmarks for an organisation’s progress in using e-rostering software. These standards outline the processes and systems needed to enhance staff deployment and boost workforce flexibility, significantly impacting overall productivity as a result.
Challenge #1 – Manual roster management
One of the most significant barriers to boosting NHS rostering productivity is the excessive time rota coordinators are forced to spend manually creating schedules, which can result in duplicated data, errors and inefficiencies. Clinicians’ preferences can’t easily be taken into account, leading to the creation of generic rotas that can impact staff morale. Ensuring compliance with regulatory requirements and maintaining minimum staffing levels becomes a manual and complex task.
As a result of restrictive rostering technology, rota coordinators frequently handle a high volume of leave requests and last-minute shift vacancies, leading to stress and imbalanced shift distribution amongst clinicians. The manual handling of these issues often requires additional meetings or communication to resolve conflicts, consuming valuable time. This lack of transparency and perceived unfairness in shift allocation can undermine trust between staff and management, exacerbating daily pressures.
Manual rostering on traditional systems can be error-prone and inefficient, making it a challenging ask for those responsible for increasing NHS rostering productivity.
Solution #1 – Preference-based rostering
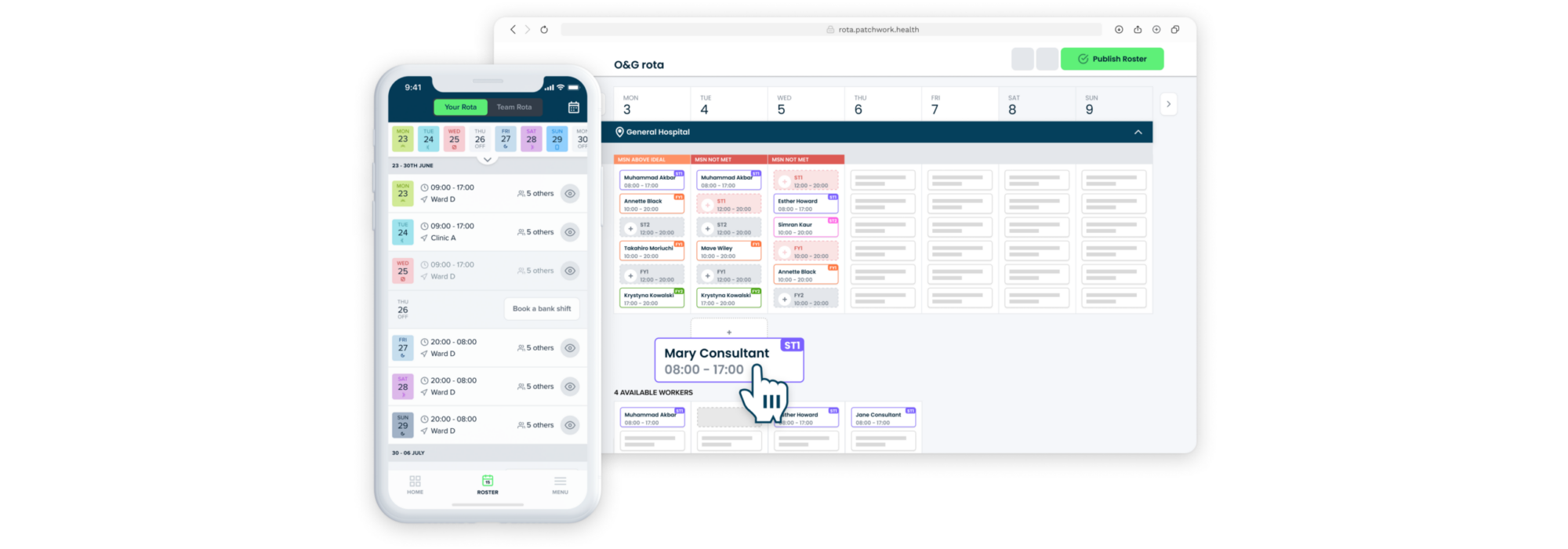
Streamlined roster creation
With effective self-rostering functionality, coordinators can create blank, draft rosters for customisable timeframes and invite staff to submit their shift preferences. The process is clearly communicated to ensure fairness, with a well-defined window for submitting preferences – this streamlined approach ensures that the initial roster creation is both efficient and accurate, minimising errors and the need for constant revisions. As a result, rota coordinators can focus on more strategic tasks rather than getting overly bogged down in administrative details. This improved workflow enhances overall productivity by reducing the time spent on roster management, improving staff satisfaction, and ensuring that shifts are covered effectively and in a way that supports the team’s well-being. Find out more here.
Automated shift allocation
Patchwork Rota algorithmically assigns shifts based on several factors:
- Compliance and regulatory requirements: ensuring all shifts meet necessary standards.
- Minimum staffing numbers (MSN): maintaining safe staffing levels.
- Scheduled leave and leave requests: factoring in previously approved time off.
- Submitted preferences: aligning shifts with staff availability and preferences.
This automation reduces the administrative burden on rota coordinators and ensures that initial allocations are balanced and compliant.

Flexibility for rota coordinators
After the initial allocations, rota coordinators can make adjustments before finalising the roster. This combination of automation and manual oversight ensures optimal shift distribution while retaining flexibility.
Benefits for staff and management
- Time savings: no need for staff to self-assign shifts or attend extra meetings for adjustments. This streamlined process saves time and reduces stress for everyone involved.
- Fairness and transparency: clear communication and fair distribution of shifts foster a positive work environment and improve relationships between clinicians and rostering teams.
- Enhanced governance: service managers gain better oversight, ensuring safe staffing levels and high standards of patient care.
By automating this aspect of roster management, systems like Patchwork Rota significantly boost organisational productivity. Rota coordinators spend less time on administrative tasks, staff experience greater control over their schedule, and overall, the system supports effective workforce management. Patchwork Rota’s new workflow offers a more efficient, fair, and productive approach to rota management, ensuring better outcomes for both clinicians and the managers in charge of the process. Two of our partners saw huge decreases in the amount of time they were spending building rosters – in one case we saw the process go from 8 hours down to 30 minutes a month.
Challenge #2 – No visibility of true staffing demand
Without a rostering system that facilitates evidence-based staffing (i.e. a structured way of mapping staffing resource against patient need), organisations risk overstaffing and understaffing, compromising both efficiency and patient care.
With most e-rostering systems, shifts aren’t aligned with actual service demand, making it difficult to deploy staff effectively. This results in rigid schedules that create a surplus of staff in some areas, and shortages in others. Consequently, organisations frequently broadcast vacancies to temporary workers, incurring unnecessary costs and underutilisation of their existing workforce.
Without an integrated system, rota coordinators struggle with double data entry and lack of oversight, making the rostering process complex and time-consuming. With assumptions or generic rota patterns often leading to constant tweaking, NHS rostering productivity is hampered.
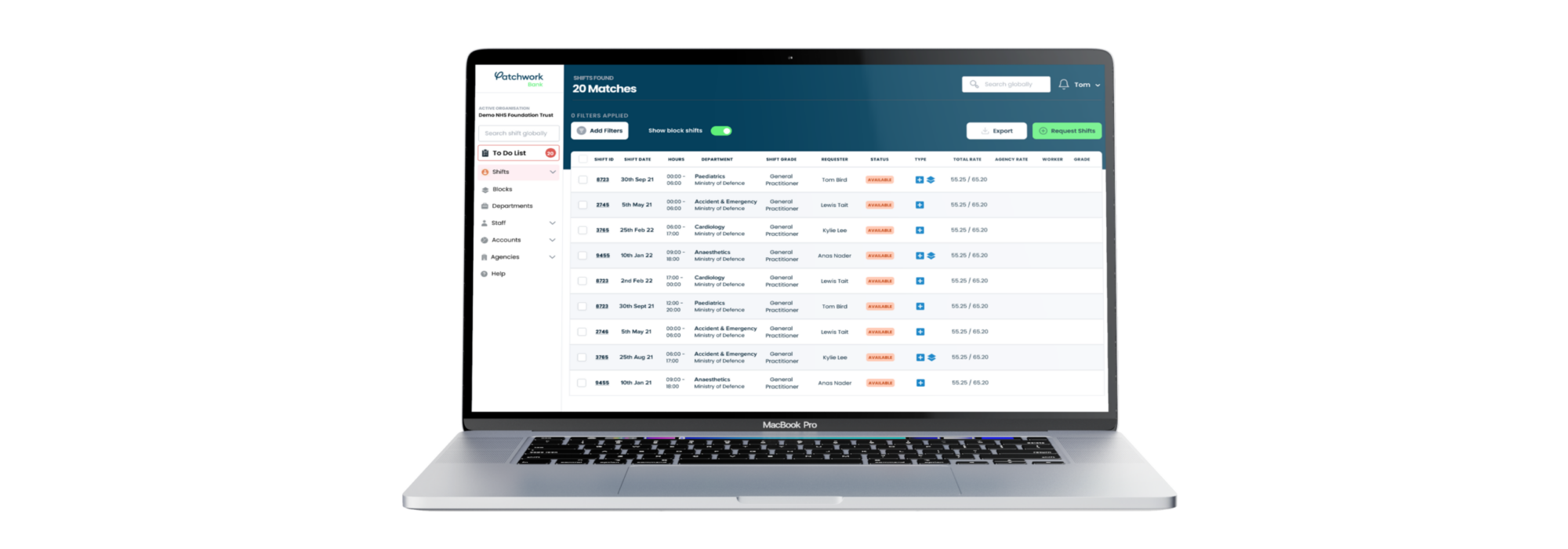
Solution #2 – Integrated service plans
Rostering systems that integrate service plans into the scheduling process enable organisations to deploy staff based on what is truly needed, by allowing for an evidence-based calculation of minimum and ideal staffing numbers. This removes any guesswork when building rosters, as service requirements are surfaced clearly at the start of, and during, the process.
With every shift mapped to true service demand, rostering teams can easily identify opportunities for inter and intra-departmental redeployment, amending staff schedules from areas of surplus to understaffed activities – utilising an organisation’s workforce in the most productive way. This can also reduce the unnecessary broadcasting of vacancies to temporary workers when a substantive clinician could have instead been redeployed, saving costs without compromising safe staffing levels.
By integrating service plans into Patchwork Rota, rota coordinators gain instant access to all the critical information they need, cutting out manual cross-checking and reducing the risk of administrative errors or last-minute schedule changes. This streamlines staff deployment, making it more efficient and directly boosting productivity. With the system’s ability to calculate minimum staffing numbers based on actual demand, you can better match staff availability to needs, avoiding both shortages and surpluses. The enhanced visibility of planned versus actual spend also allows for real-time budget tracking, helping to control costs, especially with temporary staffing deployment. This integration not only simplifies reporting and planning but also supports smarter, data-driven decisions that increase workforce output and keep operations running smoothly.

Challenge #3 – Lack of visibility
Since the dawn of rostering in the NHS, managers have faced the challenging responsibility of overseeing the rotas of hundreds of workers, often with little to no visibility of who is working where and when. Every decision within the rostering process impacts others, yet the information needed to make these decisions is rarely surfaced or easily accessible to workforce teams. This lack of visibility can lead to significant coordination and efficiency issues.
A problem with traditional rostering systems is that critical information is often siloed. For those without access or the necessary know-how, obtaining vital details – like which consultant is covering Medicine on a Friday night – can be a nightmare. This challenge extends to clinical colleagues as well. In teams where members don’t often meet each other, such as doctors sharing the same workload but rarely rostered together, the “who’s working, how can I contact them” information is often unclear. Not knowing who you’re working with, including senior or more junior grades, can hinder team coordination and workforce output.
This lack of accessibility often results in reliance on multiple Excel sheets and paper copies to communicate basic information about who is working and how to contact them. Maintaining and updating these manual records is an arduous task, significantly reducing the productivity of managers who could otherwise focus on higher-impact items. This is the reality for rota coordinators who face an almost impossible task of staying on top of everything, without the visibility needed to manage their day-to-day duties effectively.
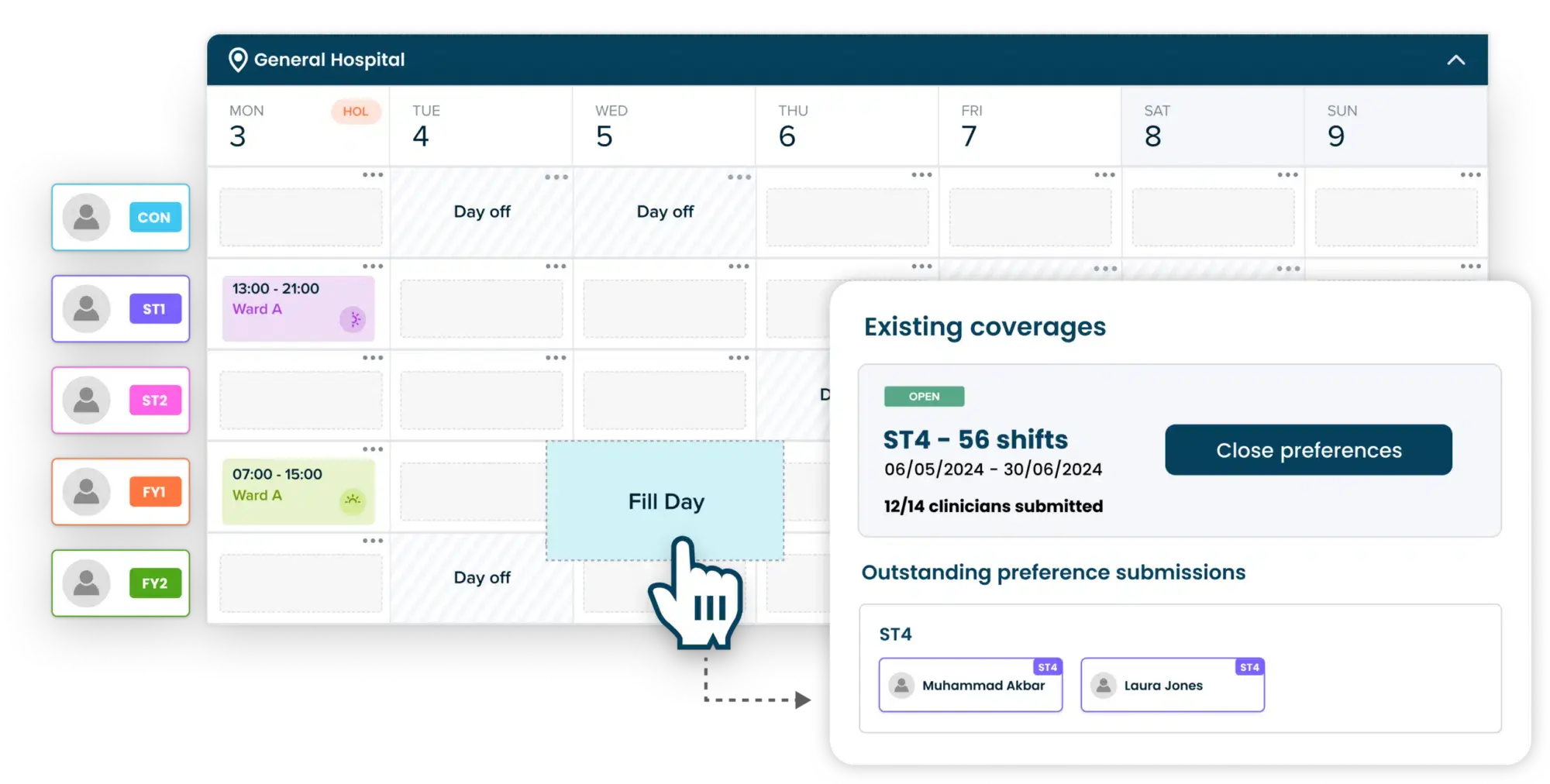
Solution #3 – Easily accessible staffing data
Increasing the data visible to staff at an organisation is crucial to supporting the entire rostering process, from staff redeployment to driving continuous improvement.
So how does data visibility boost productivity?
By giving clinicians as much visibility as possible, an organisation can hope to see the benefits of a more coordinated and productive workforce. For example, if a clinician can see who is working, it may encourage them to engage with the wider workforce, supporting shift swaps and increasing flexibility. Importantly, a flexible, engaged and supported team of clinicians is more likely to deliver excellent patient care.

Decision-making
Enhanced visibility offers significant support across day-to-day decisions. It alleviates the burden on individuals by providing clear, data-backed insights, ensuring that every decision is informed and effective. For example, when a clinician requests annual leave, a rota coordinator will be presented with a clear breakdown of the submission. No longer will they have to jump between systems or message clinicians, relieving the user of administrative tasks and enabling them to focus on higher-value work.
Continuous improvement
Another area where visibility makes a significant impact is supporting continuous improvement. By analysing collected data, organisations can identify and address issues more effectively, with data from all workforce activity supporting decision-making. This data-driven approach ensures continuous improvement, driving consistent progress and embedding productivity into the core of the organisation.
An effective e-rostering system like Patchwork Rota is essential for boosting workforce productivity in the NHS. By streamlining roster creation, integrating service plans, and enhancing data visibility, organisations can increase staffing efficiency, ensure fair and flexible scheduling, and support data-driven decision-making – all positively impacting the productivity of an organisation.